United Behavioral Health Outpatient Treatment Progress free printable template
Show details
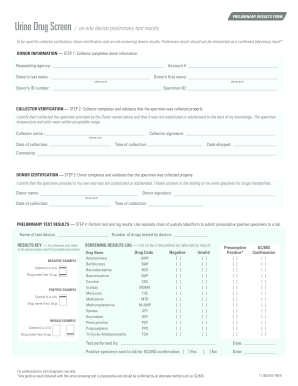
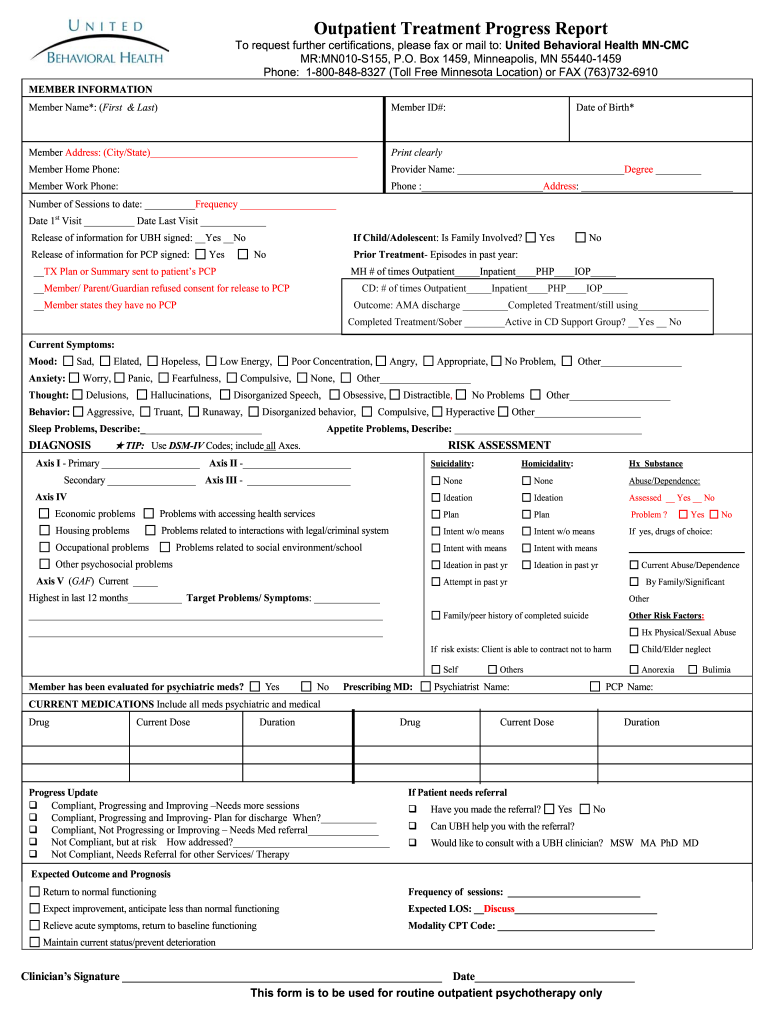
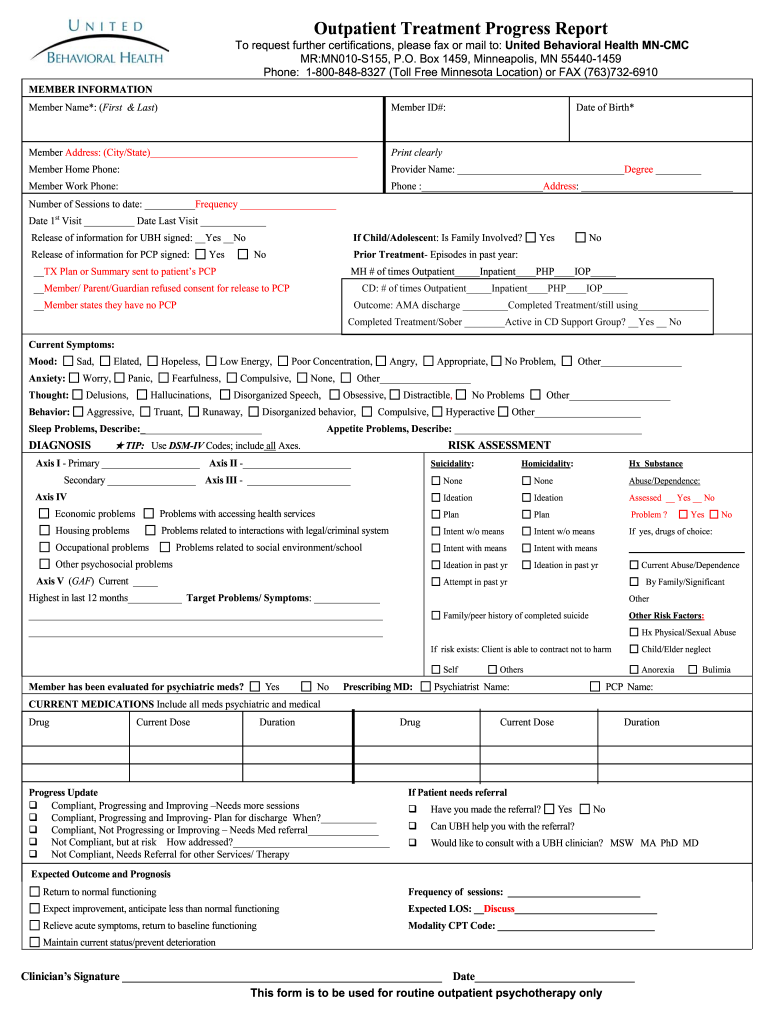
Outpatient Treatment Progress Report To request further certifications please fax or mail to United Behavioral Health MN-CMC MR MN010-S155 P. O. Box 1459 Minneapolis MN 55440-1459 Phone 1-800-848-8327 Toll Free Minnesota Location or FAX 763 732-6910 MEMBER INFORMATION Member Name First Last Member ID Member Address City/State Print clearly Date of Birth Member Home Phone Provider Name Degree Member Work Phone Phone Address Number of Sessions to date Frequency Date 1st Visit Date Last Visit...
pdfFiller is not affiliated with any government organization
Get, Create, Make and Sign substance abuse progress notes examples form

Edit your behavioral health treatment progress report form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.

Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.

Share your form instantly
Email, fax, or share your treatment progress report template form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit a substance abuse treatment progress report template current dose duration progress update and compliance online
In order to make advantage of the professional PDF editor, follow these steps below:
1
Log in. Click Start Free Trial and create a profile if necessary.
2
Prepare a file. Use the Add New button to start a new project. Then, using your device, upload your file to the system by importing it from internal mail, the cloud, or adding its URL.
3
Edit substance abuse treatment progress note template form. Rearrange and rotate pages, insert new and alter existing texts, add new objects, and take advantage of other helpful tools. Click Done to apply changes and return to your Dashboard. Go to the Documents tab to access merging, splitting, locking, or unlocking functions.
4
Save your file. Select it in the list of your records. Then, move the cursor to the right toolbar and choose one of the available exporting methods: save it in multiple formats, download it as a PDF, send it by email, or store it in the cloud.
The use of pdfFiller makes dealing with documents straightforward. Try it now!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out health outpatient progress report form

How to fill out United Behavioral Health Outpatient Treatment Progress Report
01
Begin by entering the client's personal information including name, date of birth, and identification number.
02
Fill in the date of the report and the reporting period being covered.
03
Describe the client's condition at the beginning of treatment and any notable changes to date.
04
Document the treatment goals established for the client.
05
List the interventions or treatment modalities used during this reporting period.
06
Record the client's progress towards their goals, noting successes and challenges.
07
Include any relevant observations about the client's behavior or mental state during sessions.
08
Provide recommendations for future treatment, adjustments to goals, or referrals if necessary.
09
Ensure all information is accurate and complete, then sign and date the report.
Who needs United Behavioral Health Outpatient Treatment Progress Report?
01
Mental health professionals who are treating clients and require a structured method to track progress.
02
Insurance providers who require documentation for billing and coverage decisions.
03
Clinical supervisors who need to review the effectiveness of treatment plans.
04
Clients themselves for personal records and to facilitate communication with their care providers.
Fill
substance abuse treatment progress note format
: Try Risk Free






People Also Ask about sample letter drug treatment program
What is the treatment plan process?
Treatment planning is a process in which the therapist tailors, to the greatest extent possible, the application of available treatment resources to each client's individual goals and needs. A thorough multidimensional assessment is essential to individualized treatment planning.
What is a soap note for substance use?
SOAP notes include a statement about relevant client behaviors or status (Subjective), observable, quantifiable, and measurable data (Objective), analysis of the information given by the client (Assessment), and an outline of the next course of action (Planning).
What are the components of a treatment plan?
A treatment plan will include the patient or client's personal information, the diagnosis (or diagnoses, as is often the case with mental illness), a general outline of the treatment prescribed, and space to measure outcomes as the client progresses through treatment.
What are some treatment goals for substance abuse?
Example treatment goals include: Eliminating substance use. Addressing the root cause of the addiction. Developing healthy stress management techniques. Creating a support system. Learning how to communicate emotions effectively. Maintaining a healthier lifestyle. Repairing damaged relationships.
What are the 4 parts of a treatment plan?
There are four necessary steps to creating an appropriate substance abuse treatment plan: identifying the problem statements, creating goals, defining objectives to reach those goals, and establishing interventions.
How to write progress notes for substance abuse treatment?
Sample Progress Notes for Substance Abuse Counseling Patient information: Include patient name, diagnosis, medication, mental health history and other relevant details about their substance abuse or session details. You may also include their demographic information, moods, behaviors and symptoms.
Our user reviews speak for themselves
Read more or give pdfFiller a try to experience the benefits for yourself
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I make changes in substance abuse progress notes pdf?
pdfFiller not only lets you change the content of your files, but you can also change the number and order of pages. Upload your behavioral outpatient progress to the editor and make any changes in a few clicks. The editor lets you black out, type, and erase text in PDFs. You can also add images, sticky notes, and text boxes, as well as many other things.
How do I edit drug rehab application form in Chrome?
Install the pdfFiller Google Chrome Extension in your web browser to begin editing addiction recovery progress note template and other documents right from a Google search page. When you examine your documents in Chrome, you may make changes to them. With pdfFiller, you can create fillable documents and update existing PDFs from any internet-connected device.
How do I fill out the drug rehab certificate of completion template form on my smartphone?
The pdfFiller mobile app makes it simple to design and fill out legal paperwork. Complete and sign drug rehab completion letter sample and other papers using the app. Visit pdfFiller's website to learn more about the PDF editor's features.
What is United Behavioral Health Outpatient Treatment Progress Report?
The United Behavioral Health Outpatient Treatment Progress Report is a document used by healthcare providers to track and document the progress of patients undergoing outpatient mental health treatment.
Who is required to file United Behavioral Health Outpatient Treatment Progress Report?
Healthcare providers, particularly those involved in the outpatient treatment of behavioral health patients, are required to file the United Behavioral Health Outpatient Treatment Progress Report.
How to fill out United Behavioral Health Outpatient Treatment Progress Report?
To fill out the report, providers need to complete sections that detail the patient's treatment objectives, progress made, therapeutic techniques used, and any changes to the treatment plan, ensuring all information is accurate and up-to-date.
What is the purpose of United Behavioral Health Outpatient Treatment Progress Report?
The purpose of the report is to monitor a patient's progress in therapy, facilitate communication among treatment providers, and ensure that the treatment is effective and aligned with the patient's needs.
What information must be reported on United Behavioral Health Outpatient Treatment Progress Report?
The report must include the patient's demographic information, treatment goals, progress towards those goals, any interventions provided, and recommendations for future treatment.
Fill out your United Behavioral Health Outpatient Treatment Progress online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.
Sample Progress Notes For Substance Abuse is not the form you're looking for?Search for another form here.
Keywords relevant to behavioral health mental health progress note template
Related to proof drug rehab completion letter
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.